An Interesting ECG Case
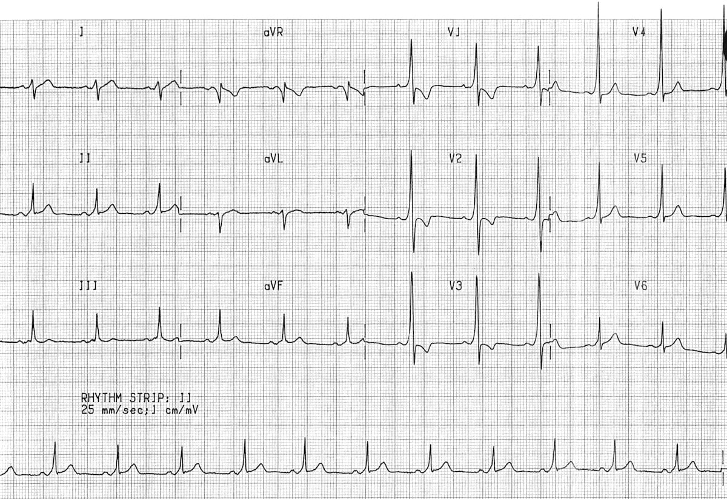
36-year-old male calls 911 for palpitations and mild chest discomfort following a stressful meeting at work. He denies syncope but feels lightheaded. No significant medical history, but he recalls being told he a minor ECG abnormality following a medical exam years ago. He was told to report any significant palpitations. Vitals: BP 132/76, HR 132 bpm, afebrile. EMS records the following ECG:
Is this a STEMI?
No, this ECG shows features of Wolff-Parkinson-White (WPW) Syndrome, which can sometimes mimic STEMI:
• Short PR interval (< 120 ms)
• Delta wave: slurred upstroke in the QRS complex
• Tall R wave V1-3
• Wide QRS complex (> 120 ms)
• ST-segment depression, especially in leads V1-3—raising concern for posterior STEMI
Key Teaching Points
• WPW can mimic ischemia on ECG, especially in posterior leads.
• Avoid misinterpretation—thrombolysis or cath lab activation may be inappropriate.
• The clinical context (young patient, stable vitals, known history) is crucial.
Management
• Assessment of possible ACS with consideration of presenting symptoms, serial ECGs, cTNT measurement and bedside echo may assist in unclear cases.
If supraventricular tachycardia, in stable patients: vagal maneuvers or procainamide (in consultation with cardiology). Electrical cardioversion for unstable patients.
• Electrophysiology (EP) referral is warranted.
• Consider ablation of accessory pathway as definitive treatment.