An Interesting ECG Case
56-year-old male presents to the ED with 3 hours of chest pain, 2 months after minimally invasive mitral valve repair. Pre-op angiography showed 40% proximal RCA stenosis; no CABG.
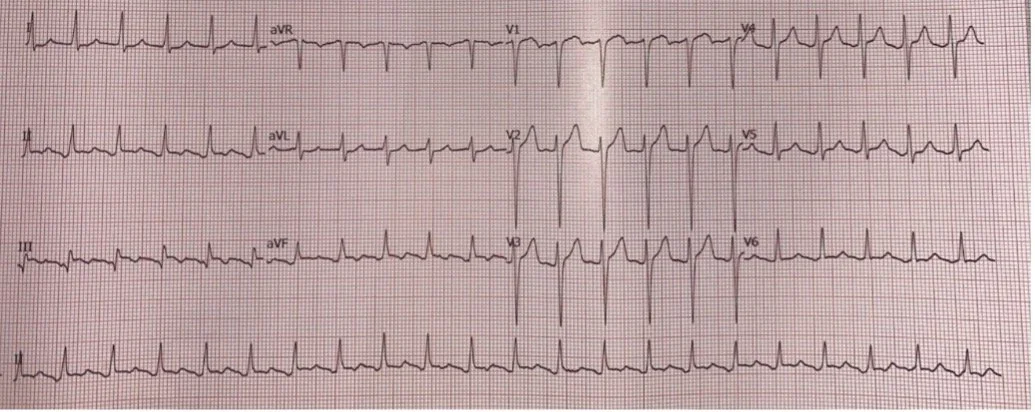
His pain is sharp and worse with deep inspiration. Vitals are stable. Here is his ECG:
The ECG shows a supraventricular tachycardia at 136 BPM. There is mild ST elevation in III with borderline ST elevation in and aVF.
Is he having a STEMI?
No—this is not an inferior STEMI.
This ECG shows:
Atrial flutter with 2:1 AV conduction, giving a regular narrow-complex tachycardia
Flutter waves distorting the baseline, especially in the inferior leads
Apparent inferior ST elevation created by flutter waves, not true ST-segment shift
When measured from the true isoelectric baseline (between flutter waves), ST segments in II, III, and aVF are essentially isoelectric, without convincing reciprocal changes
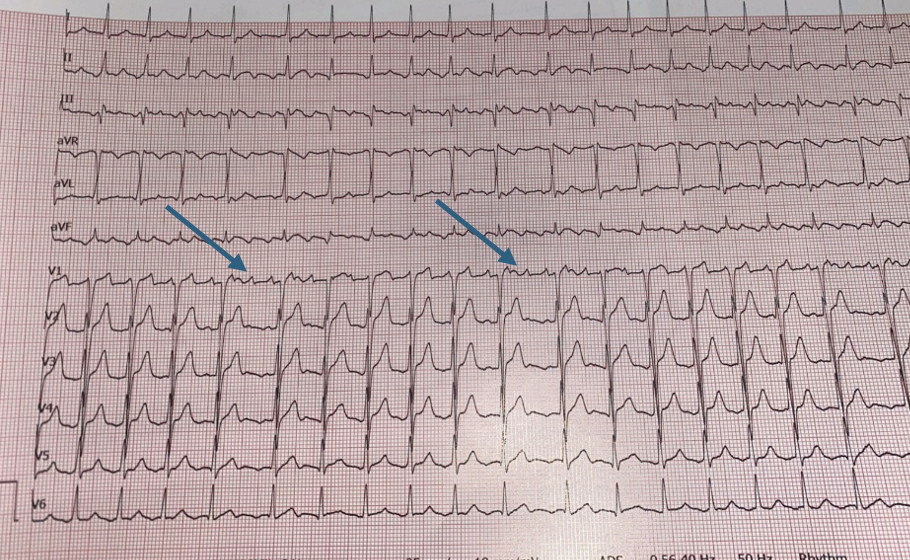
The diagnosis became clear when:
Focused history confirmed the pain was pleuritic, not typical for MI
A rhythm strip during adenosine produced transient AV block, unmasking classic flutter waves
The final diagnosis: atrial flutter with post-operative pericarditis, mimicking an inferior STEMI.
Clinical Significance
Atrial flutter after cardiac surgery is common and can:
Distort the ST segments and simulate inferior STEMI
Post-op pericarditis:
Causes pleuritic, sometimes positional chest pain
May have subtle or obscured ECG changes when flutter is present
Management Lessons
Be cautious about activating Code STEMI for borderline inferior ST elevation when:
Pain is pleuritic/positional, and
The rhythm is suspicious for flutter or other atrial activity
Adenosine (when safe) can:
Reveal atrial flutter by inducing transient AV block
Allow accurate reassessment of true ST segments
Take-home: In post-surgical patients, always interpret ST segments in the context of the rhythm and chest pain characteristics—atrial flutter can convincingly mimic an inferior STEMI.